Moles, also known as nevi, are pigmented skin growths caused by clusters of melanocytes, which are pigment-producing cells. They may appear flat or raised and can vary in colour from light brown to nearly black. Moles are very common, and most adults have between 10 to 40 moles on their bodies.
Some moles are present from birth, while others appear gradually over time, often during childhood or adolescence. In most cases, moles are harmless and do not require treatment. However, changes in size, shape, or colour may indicate a risk of skin cancer and should be evaluated by a dermatologist.

| Type of Mole | Features |
|---|---|
| Acquired Nevi |
|
| Congenital Nevi |
|
| Compound Nevi |
|
| Intradermal Nevi |
|
| Junctional Nevi |
|
| Dysplastic (Atypical) Nevi |
|
The exact cause of mole formation is not fully understood. But genetics and environmental factors, particularly sun exposure, play a role. Some of the key contributing factors include:
Benign moles typically have a consistent and predictable appearance. As such, knowing what normal moles look like helps you detect any changes that may warrant medical attention.
These characteristics include, but are not limited to:
Although moles can form in anyone, there are certain individuals who are more predisposed due to several factors. The groups that are at higher risk are:

Moles consist of melanocytes, the same cells involved in melanoma. Although most moles remain stable, a small number may undergo changes that lead to uncontrolled cell growth.
Melanoma arises when melanocytes become cancerous and begin to multiply abnormally. This can occur within an existing mole or develop as a new lesion.
Some of the triggers for mole-to-melanoma transformation may include:
About 25% to 30% of melanomas arise from pre-existing moles, with the rest appearing as new lesions. This is why routine monitoring and early intervention are critical.
Most moles are completely harmless and do not change throughout your lifetime. However, certain signs may suggest that a mole is becoming atypical or possibly cancerous.
You should consult a dermatologist if a mole:
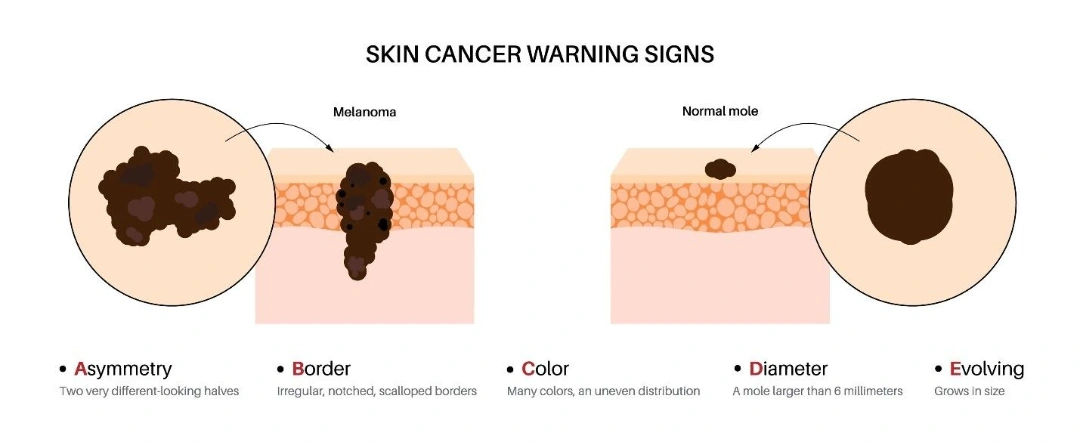
The ABCDE rule is a simple but effective tool for identifying potentially suspicious moles:
When it comes to diagnosing moles, we use a structured and meticulous approach to accurately assess and diagnose moles. Our goal is to differentiate between harmless and suspicious lesions to ensure safe and timely treatment.
Our diagnostic process includes:
Mole removal may be suggested for medical, aesthetic, or practical reasons. Even benign moles can sometimes cause discomfort or interfere with daily life.
Some of the common reasons for mole removal include:
Before any removal, our dermatologist will perform a thorough assessment to ensure the right technique is chosen based on the mole's type, depth, and location.

At Cove Aesthetic Clinic, mole removal is a safe and straightforward outpatient procedure performed by trained medical professionals. The appropriate method depends on the mole’s type, size, depth, location, and whether it shows any signs of potential malignancy.
Each removal technique is selected carefully to balance clinical effectiveness, aesthetic outcomes, and, when needed, histological assessment.
This is the most comprehensive method and is often used for moles that are deep, large, or clinically suspicious.
A common method for removing raised or protruding moles that are benign in appearance.
This involves the use of a small, circular tool to remove both the mole and a column of surrounding tissue.
Laser mole removal is a non-invasive option for moles that are flat, superficial, and benign.
This method involves freezing the mole using liquid nitrogen, which destroys the pigmented cells.
Electrocautery uses heat generated by an electric current to burn and destroy mole tissue.

Whether you are concerned about a changing mole or simply wish to remove one for cosmetic reasons, expert evaluation is the first step. At Cove Aesthetic Clinic, our experienced team offers safe, effective mole assessment and removal tailored to your needs, with a focus on both medical accuracy and aesthetic outcomes.
Book a consultation with us today to have your moles assessed and explore the most suitable treatment options for your skin.
No. Most moles are benign and do not pose a health risk. However, certain types, such as dysplastic or atypical moles, have a higher chance of becoming cancerous and should be monitored regularly.
Only a medical professional can confirm whether a mole is cancerous, usually through a biopsy. However, signs such as changes in size, shape, colour, bleeding, or itching may warrant immediate medical attention. The ABCDE rule is a helpful guide.
New moles can form due to hormonal changes, sun exposure, or genetics. If a new mole appears and looks unusual or changes rapidly, it is best to have it evaluated.
Yes, hormonal changes during pregnancy can cause existing moles to darken or new ones to form. These changes are usually benign, but it is best to have any rapidly changing moles checked by a dermatologist.
You may not be able to prevent all moles, especially if you are genetically predisposed. However, limiting UV exposure, wearing sunscreen daily, and avoiding tanning beds can help reduce the development of new moles.
No, mole removal should never be attempted at home. DIY methods can lead to incomplete removal, infections, scarring, or worse—missed diagnoses of skin cancer. Always seek professional evaluation and removal from a trained medical provider.
Mole removal procedures are generally not painful. Local anaesthesia is applied to numb the area before removal. You may feel mild pressure during the procedure, and some tenderness or redness afterwards, which typically resolves within a few days.
Some scarring is possible, depending on the mole’s size, depth, and the removal method used. However, our dermatologists take great care to minimise scarring, especially for facial or visible areas. Over time, most scars fade significantly.
Laser removal is safe and effective for treating small, flat, non-cancerous moles. However, it is not recommended for suspicious moles, as no tissue is left behind for biopsy. Our dermatologist will determine if it is appropriate for your case.
In some cases, yes. If a mole is not completely removed, especially with superficial methods like shaving, it may regrow. Complete surgical excision reduces the likelihood of recurrence.
Yes. Many patients choose to remove moles that are visible, raised, or bothersome. Cosmetic mole removal is safe when performed by a qualified medical professional and typically leaves minimal scarring.
Yes. Mole removal is safe for children and teens when medically indicated or requested for cosmetic reasons. Evaluation by a dermatologist is essential before proceeding with removal in younger patients.
Healing times vary depending on the technique used and the individual’s skin type. In most cases, surface healing takes 7 to 10 days. Complete healing and scar fading can take several weeks to a few months.















